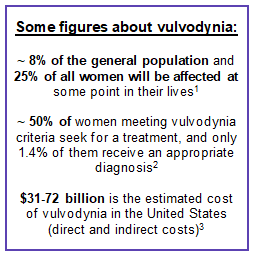
Vulvodynia: a little-known but highly impacting condition for many women around the world

According to a study conducted by Alcimed, most patients with vulvodynia would consult about 10 different healthcare professionals over several years before receiving the correct diagnosis associated to these symptoms.
Lyon, May 10, 2019 – The word vulvodynia comes from “vulvo” meaning vulva and “dyny” meaning pain, which literally means “pain in the vulva”. However, since 2003, vulvodynia has been more broadly defined by the International Society for the Study of Vulvovaginal Disease (ISSVD) as “chronic vulvar discomfort, most often a type of burn, without relevant visible lesions and not associated to a clinically identifiable neurological disease”.
 Vulvodynia is part of the Medically Unexplained Symptoms (MUS), i.e. not related to an identifiable organic disease. Other, more well-known examples are: fibromyalgia, interstitial cystitis, irritable bowel syndrome, temporomandibular joint dysfunction, chronic fatigue syndrome, etc. In addition, 50% of women with vulvodynia have at least two associated MUS.
Vulvodynia is part of the Medically Unexplained Symptoms (MUS), i.e. not related to an identifiable organic disease. Other, more well-known examples are: fibromyalgia, interstitial cystitis, irritable bowel syndrome, temporomandibular joint dysfunction, chronic fatigue syndrome, etc. In addition, 50% of women with vulvodynia have at least two associated MUS.
The causes of vulvodynia are still not well-known and poorly defined. Genetic factors could predispose people to this disease, local inflammations could play an inductive role (such as a Candida albicans infection), psychosocial environmental factors would also be involved as well as a history of physical, psychological or sexual violence that multiplies the risk of developing vulvodynia by 4 to 6.
The condition is mainly characterized by severe pain, which can be either generalized or localized (vestibulodynia, clitorodynia, hemivulvodynia, etc.). In both cases, they can be provoked (by sexual contact, non-sexual contact, or both), unprovoked (spontaneous pain) or mixed (provoked and unprovoked). These pains are most often described as burning, but other sensations are also expressed as throbbing, pinching, stinging, soreness, dryness, etc.
Problems related to the pathology
The diagnosis of vulvodynia is based on a clinical examination and additional tests to rule out any possible infection that could explain the pain of the vulva (candidiasis, herpes, etc.). However, a lack of knowledge about the pathology leads to a misdiagnosis and a delay in diagnosis ranging from a few months to several years. Most patients consult multiple doctors or specialists and undergo many tests before they are diagnosed correctly. Diagnostic errors are an extremely common challenge, as is the problem of not being taken seriously.
Furthermore, many disorders are associated with vulvodynia. In addition to severe physical pain (on a scale of 1 to 10, with 1 being associated with “little pain” and 10 with “maximum pain imaginable”), patients interviewed in a study reported that their pain was chronic and never went below 5 out of 10. The psychological impact and the impact on the quality of life are therefore very important. Feeling ashamed, losing self-confidence, depression, difficulty or even inability to perform certain activities (playing sports, walking, sitting too long, having sex, etc.) are significant limitations associated with vulvodynia.
Existing treatments
To date, no specific treatments exist yet; however, many solutions (topical, oral and other therapies like physiotherapy and psychotherapy) are available and are often combined to treat each patient on a case-by-case basis. Three main types of treatments can be distinguished:
-Medicinal: local anesthetic or analgesic drugs, oral painkillers, antiepileptic drugs, antidepressants, psychotropic drugs.
-Non-medicinal: sweet almond oil, baths, etc.
-Other therapies: surgery (injection into the pudendal nerve), laser therapy, neurostimulation, physiotherapy, psychotherapy, yoga, relaxation, meditation, etc.
A patient’s journey to find her personal best solution is often long and tiring. Indeed, for the majority of them, no solution works and this whole process of trial and error is a psychological ordeal as much as a financial break.
Faced with patients’ high level of suffering and the high prevalence of this disease, many associations exist and serve as vectors of information, intermediaries or mediators.
For example, the “Associazione Italiana Vulvodinia Onlus” association in Italy and “Les Clefs de Vénus” in France its missions are informing about chronic pain and helping women suffering from it.
What are the future projections?
Tomorrow’s challenge will be to train and inform healthcare professionals in order to fight against diagnostic errors, the lack of serious symptom management and the loneliness of patients; but also to promote the search for new treatments to help these suffering women.
1 Therapeutics in Dermatology, A reference textbook in dermatology: “VULVODYNIA”, 29 February 2016, by MOYAL-BARRACCO M. & DO PHAM G.
2 “Prevalence and demographic characteristics of vulvodynia in a population-based sample”, February 2012, Reed et al.7
3 “Vulvodynia: Definition, Prevalence, Impact, and Pathophysiological Factors”, December 20, 2015, Caroline F. Pukall
Do you have an exploration project?
Our explorers are ready to discuss it with you