The CAR-T cell revolution: The funding puzzle
With impressive results, particularly where conventional treatments have failed, CAR-T cells represent a real revolution in onco-hematology care. Two treatments are already available in the United States and are about to arrive in Europe. Alcimed, a consulting company specialized in innovation and the new businesses, has investigated this expensive therapy whose next challenge is undeniably its financing.
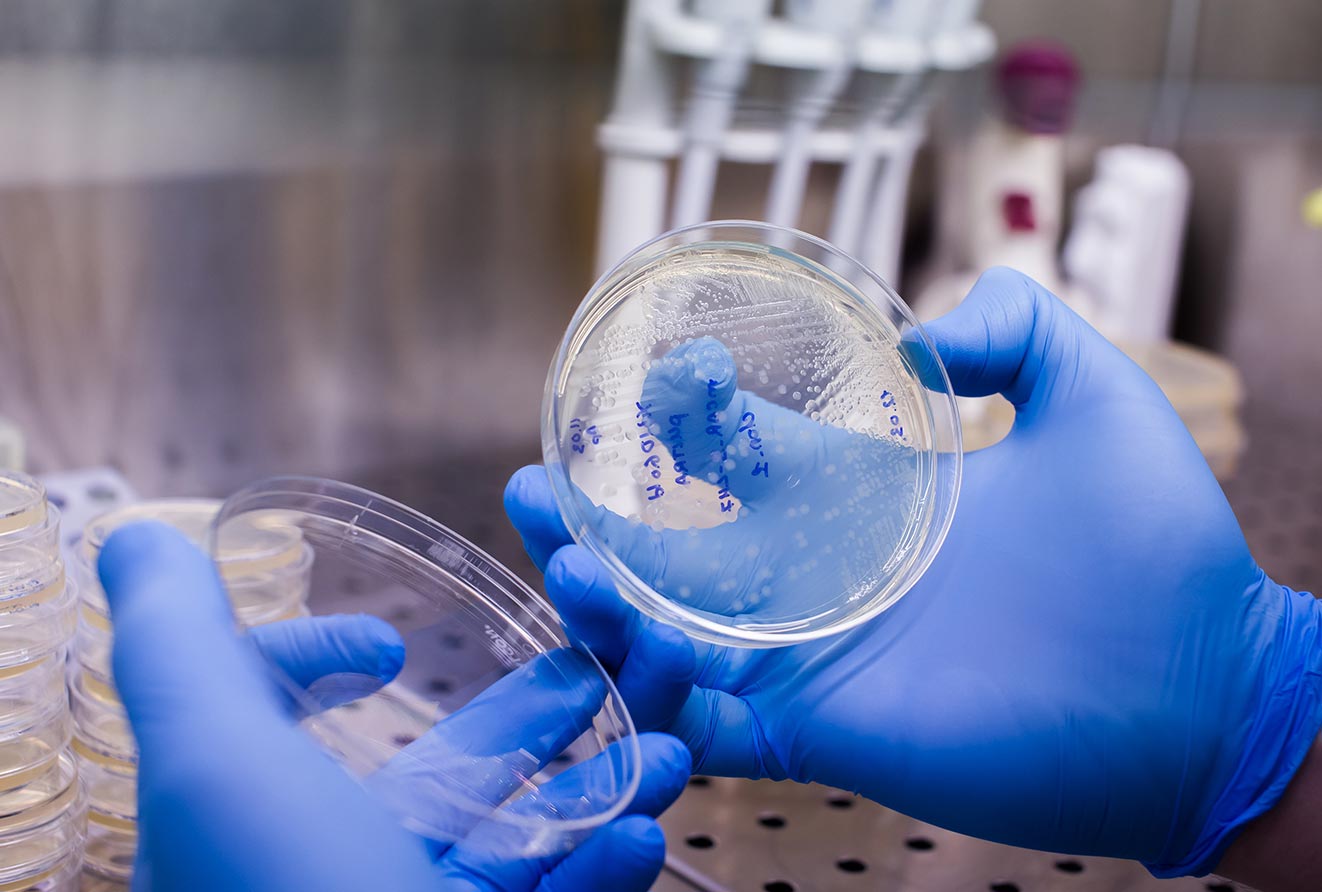
Immunotherapy, between cell therapy and gene therapy
Using a patient’s T lymphocytes and genetically modifying them to treat cancer has now become possible! The T cells, whose role is to ensure immune response, do not always recognize cancer cells that conceal themselves using various mechanisms, allowing for the formation of tumors. CAR-T cells are modified T lymphocytes that are no longer susceptible to those diversion techniques as they contain a specially designed receptor that recognizes an antigen specific to cancer cells. In order to obtain such cells, the patient’s T lymphocytes are sampled, genetically modified in vitro (so that they express the artificial chimeric receptor), multiplied and reinjected into the patient: resulting in Chimeric Antigen Receptor-T cells (CAR-T cells).
A trending immunotherapy
With impressive rates of complete remission (up to 90%) in patients for whom none of the conventional treatments had worked, CAR-T cells have not failed to attract the industry with several companies positioning themselves on this immunotherapy. Although many treatments are in development, two have already obtained a marketing authorization in the United States for an aggressive form of leukemia (Novartis Kymriah® in August 2017) and non-Hodgkin lymphoma (Gilead Yescarta® in October 2017, Kymriah® in May 2018). At the end of June, the Committee for Medicinal Products for Human Use (CHMP) in Europe issued a positive opinion on the marketing of these immunotherapies. This will be forwarded to the European Commission, which has the decision-making power on the issuance of marketing authorizations (MA) at the level of the European Union. Once these MAs have been obtained, it will be up to each member country to set the price and reimbursement terms. Last July in France, the ‘Agence Nationale de Sécurité du Médicament (ANSM)’ issued temporary authorizations for these treatments in order to accelerate access pending the issuance of marketing authorizations and price negotiations.
An expensive therapy
Pricing is an important issue that cannot be underestimated. In the United States, Yescarta® and Kymriah® are priced at $373,000 and $475,000 respectively for a single injection of CAR-T cells, placing them among the most expensive drugs ever made. In addition, this cost is independent of related costs such as hospital stays, specialist consultations, etc. However, where some think only in terms of cost, it is rather the value provided by this type of therapy that should be considered to understand the rationality of the price. Because, if CAR-T cells allow a lifetime remission of the patient, their price will largely compensate the costs usually generated by relapses and subsequent treatments, especially since these therapies partially target young patients. Medico-economic studies are now needed to convince health agencies and private insurance companies.
But where can we find the funds to finance these therapies? The question is a thorny one, especially since these therapies could eventually be extended to many other indications. In the United States the CMS (Center for Medicare and Medicaid Services – the body that sets health care reimbursements for the two insurances) has opted for hospital reimbursement of between $400,000 and $500,000. However, this coverage only seems viable by reallocating the budget of other therapies and/or increasing the prices of health insurance contributions.
Towards new financial models …
The current situation is leading to the development of new payment models as the first lever to limit costs for health systems. For example, Novartis has entered into a full refund agreement with the CMS in the event of a one-month treatment failure. This system, called “performance-based payment”, has already existed for several years for expensive therapies and allows health systems to pay pharmaceutical companies only in the event of a patient’s remission following treatment. Another possibility would be to spread the payment over several years, and stop it as soon as the treatment ceases to be effective: this model is particularly suitable for diseases where the relapse rate is not negligible. Thus, for a treatment at €500,000, the health system could pay the manufacturer €100,000 for the first year, then €50,000 for each additional year if the patient is cured. In the event of a relapse, the health system would then stop payments, thus limiting the costs incurred for a therapy that has not proven effective in the long term. However, this model is constrained in the United States due to the extremely competitive health insurance system, which is characterized by a very short-term loyalty among insured persons. Who will be responsible for the remaining payments in the event of a change in the patient’s health insurance?
…or new production systems
A second lever to reduce the costs of these therapies would be to optimize their production process. Today, the manufacturing process of Yescarta® and Kymriah® is individualized for each patient. But what about using allogeneic CAR-T cells, i.e. cells produced from T cells from healthy donors, instead of individually sampling the patient’s T cells? Cellectis has chosen this path, aiming at manufacturing CAR-T cells industrially. At the same time, CRISPR Therapeutics also aims to offer industrially produced CAR-T cells, genetically modifying them using the CRISPR molecular scissors. The price of such ‘industrially’ produced cells remains to be seen.
“Today, even if the problem of sustainable financing has not yet been solved, CAR-T cells are undoubtedly among the most promising therapies to overcome cancer.” concludes Delphine Bertrem, Head of Alcimed’s Healthcare business in Paris. It remains uncertain whether these new approaches will be sufficient to democratize the use of these therapies.