What is a lung transplant?
Lung transplantation is a complex surgical procedure designed to replace a failing lung with a healthy organ from a deceased donor. This procedure is often the last option for patients suffering from advanced lung diseases such as cystic fibrosis, interstitial lung disease, chronic obstructive pulmonary disease (COPD) or pulmonary arterial hypertension.
Compared with kidney transplantation, for example, this procedure is carried out only after a donor has died and as a last resort for the patient, which explains the low number of procedures carried out each year.
The success of lung transplantation depends on several factors, including the immunological compatibility between donor and recipient, the quality of the donor organ and the time elapsed between removal and transplantation.
What is ex vivo technology?
Ex vivo technology plays a part in the lung transplant process by enabling lungs to be preserved and rehabilitated outside the human body. Instead of transporting the organ immediately after removal, surgeons can keep it alive in a controlled environment using special preservation solutions. This ex vivo process offers many advantages, including extending the time that organs remain viable, allowing organs to be assessed and treated prior to transplantation, and reducing the risks associated with rejection.
The advantages of ex vivo technology for lung transplantation
A solution to the problem of organ shortage
Firstly, ex vivo technology offers a solution to the pressing problem of organ shortage by increasing the length of time that lungs can remain viable, thereby widening the window for finding compatible donors. In addition, the ex vivo process allows medical teams to assess and improve the quality of organs prior to transplantation, thereby reducing the risk of post-operative complications.
The ability to detect and correct potential lesions
Ex vivo technology also enables targeted treatment of organs, such as the detection and correction of potential lesions. Lungs can be perfused with nutrient solutions and specific drugs to treat identified problems, optimizing their function before being transplanted.
Improving organ stability
Technical advances in ex vivo technology have considerably improved the stability of organs during the preservation period. Modern ex vivo perfusion systems allow meticulous control of temperature, pressure and composition of perfusion fluids, creating optimal conditions for maintaining lung vitality. These advances reduce the risk of cell damage and organ dysfunction during the critical period between removal and transplantation.
What are the prospects for ex vivo rehabilitation of lung grafts?
Optimizing results and the use of digital technology
The future of ex vivo technology in lung transplantation lies in the ongoing optimization of outcomes. Researchers are exploring ways to improve the quality of ex vivo organ preservation and to identify reliable biomarkers for assessing lung viability prior to transplantation. This would enable more accurate selection of donor organs and help reduce rejection rates.
Researchers are also envisioning advanced computer modelling techniques to predict the behavior of organs after transplantation. By better understanding the dynamics of lung transplantation, medical teams could adjust treatment protocols and personalize post-operative care to maximize the chances of success.
Extending the scope of the technology
Beyond lung transplantation, ex vivo technology could extend its footprint to other organs, paving the way for significant advances in organ transplantation in general. Researchers are already exploring the application of this technology to the kidney, liver and heart, broadening the scope of potential benefits.
Using biotechnologies
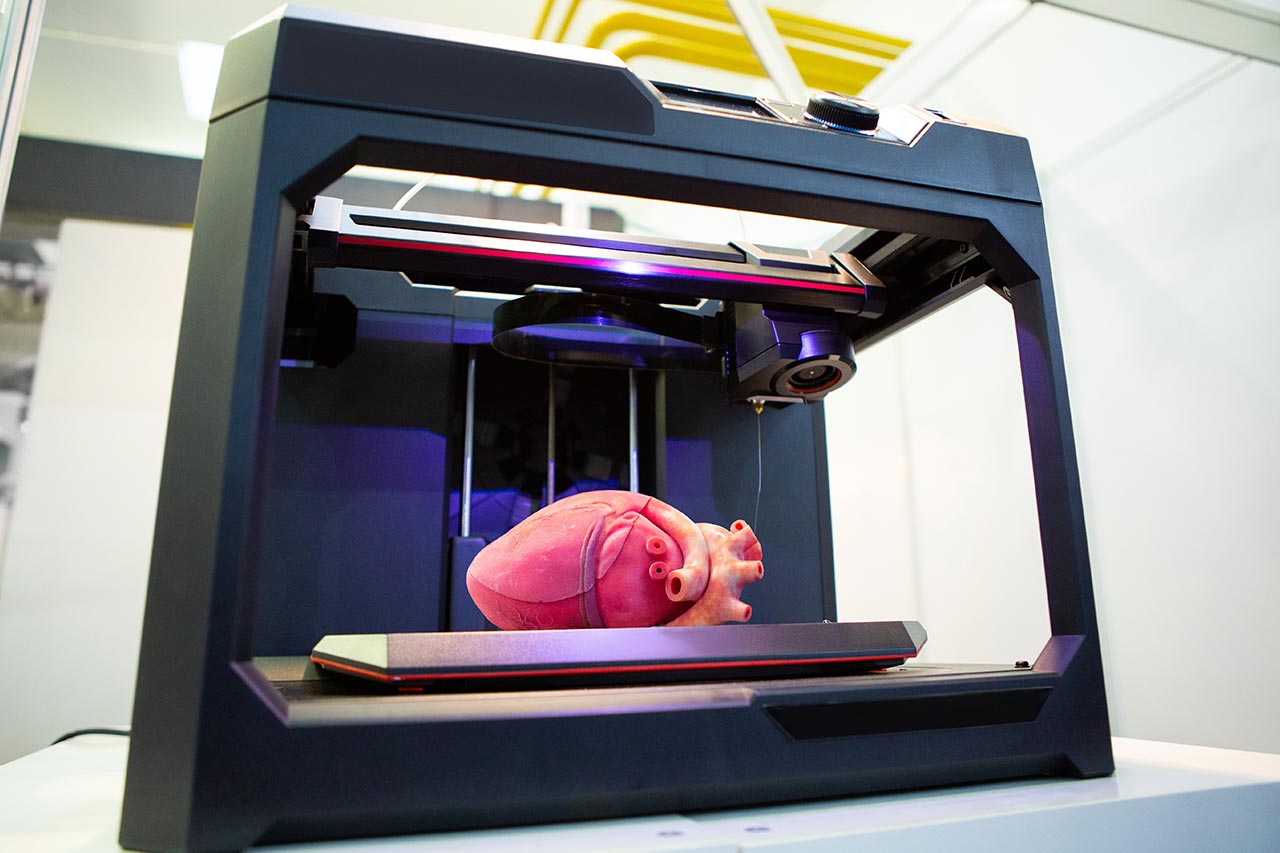
Advances in the genetic modification of organs ex vivo to improve their compatibility with recipients are conceivable. Such approaches could revolutionize transplantation by further reducing the risk of rejection and increasing the availability of compatible organs.
This biotechnology also offers the possibility of developing tailor-made organs, designed to adapt perfectly to the specific needs of each patient. While this may seem like a futuristic prospect, rapid advances in tissue engineering and genomics suggest that the creation of tailor-made organs could become a reality in the relatively near future.
Find out how our team can help you with your projects related to regenerative medicine >
The prospects for developing ex vivo technology raise ethical, logistical and practical issues such as standardization of procedures and specialist training of medical staff. Nevertheless, the potential benefits, such as increasing the number of organs available and improving post-transplant outcomes, justify continuing this research and putting it into practice.
The example of ex vivo lung transplantation, which has given hope to many patients suffering from serious lung diseases, provides a glimpse of all the prospects offered by cutting-edge medical devices. At the heart of these innovations, Alcimed can support you in your innovation projects and the development of new markets linked to the medical technologies of the future. Do not hesitate to contact our team.
About the author,
Mathieu, Consultant in Alcimed’s Innovation and Public Policy team in France