Healthcare
Impact of COVID-19 on mental health: what are the long-term consequences?
What are the expected long-term mental health consequences of COVID-19? What will be important to focus on following the crises?
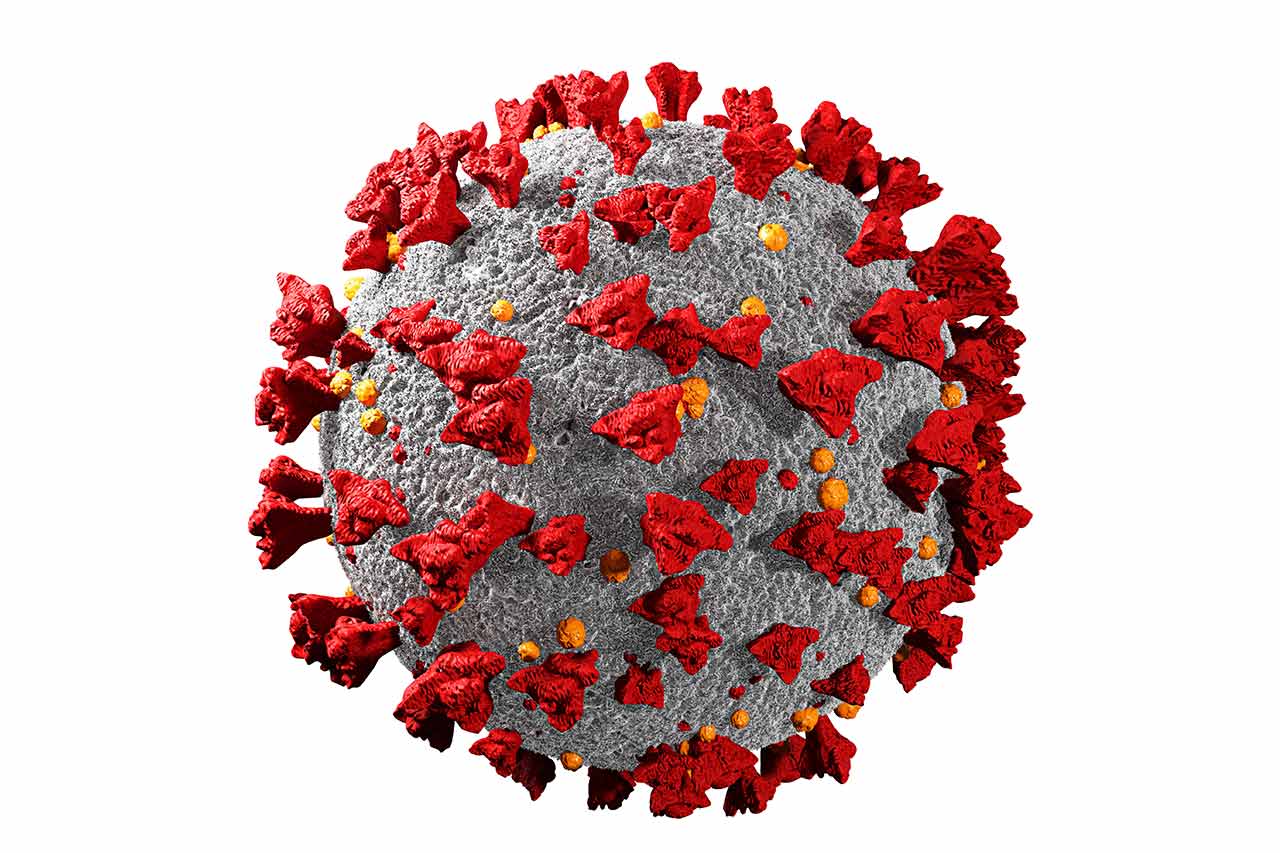
The Covid-19 pandemic is having serious effects on humanity by disrupting social,societal, educational and medical norms. Over 2,5 million people have died globally due to Covid-19 with many survivors still feeling side-effects months after getting ill. However, the side effect of Covid-19 itself is the number of the deaths that are not directly linked to the virus. In this article, we shed some light on negative effects of Covid-19 on current and future cancer patients’ quality of life.
During the multiple waves of the Covid-19 pandemic, hospital staff was facing different issues. Intensive care unit beds were heavily occupied by Covid-19 patients, which bounded massive capacities be it equipment or staff. This was even more aggravated by the fact that staff was often testing positive to Covid-19 and needed to quarantine itself. The shortfall of staff resulted in the inability to run normal service with operating roomsclosed, screening programs shortened and diagnostic procedures postponed. In turn, the detection of cancer cases was lower, and the start of treatment was delayed leading to lower quality of life and higher mortality rates in patients.
Besides diagnosis and treatment, the level of cancer management must be discussed. The world witnessed unprecedently quick adaptation of digitalization for medical care with tele-medicine at the forefront. Even though Covid-19 has driven this positive change, the usage of remote systems is biased by racial and social differences and does not seem to allow equal utilization. Personal interaction is also key during the first interactions with health practitioners in order to build trust, especially in cancer management. Even when face-to-face appointments are possible, mask-wearing can disturb communication and deteriorate trust leading to decreased outcome. In conclusion, the Covid-19 pandemic has reduced the numbers of diagnosed patients, lowered survival rates and patients’ QoL.
“Only a 3-month delay to surgery could result in >4700 attributable deaths in England across stages 1 to 3.”
Because of the issues described ealier, notably the lack of personnel to run operating rooms many non-essential but also essential surgical procedures had to be cancelled, or postponed. This affects all types of surgeries but has a dramatic effect in the field of oncology.
The numbers show that only a 3-month delay to surgery could result in >4700 attributable deaths in England across stages 1 to 3 (with variations depending on the tumor type) and the highest death rates are seen in very aggressive cancers, where even a short delay of surgery negatively impacts survival time.
For many solid tumors a 5-year survival equals cure. Before Covid-19 reports show that each cancer surgery, across all cancers, was responsible for 18 life-years gained (LYG), while a 3 months delay of surgery would drop this value to 17 LYG and a 6-month delay to 15.9 LYG.
Lastly, delays also result in patients developing advanced stages of cancer. This means not only that survival is decreased, but also subsequent treatment costs are higher. Moreover, the stage of the tumor is much later and quality of life of patients is strongly reduced.
The third way the Covid-19 pandemic is impacting quality of life and cancer case numbers is social distancing. It is now clear that many patients, lonely at home drink more alcohol, smoke more than before, don’t do sports anymore. One can easily imagine that these changed habits are the way to higher cancer cases in the (near) future as these are cancer-related health habits and absolutely the opposite of cancer prevention. In short, the Covid-19 pandemic most likely will increase number of cancer cases in the future.
In conclusion, the Covid-19 pandemic impact on cancer patients is immense, quality of life is strongly reduced and outcome is worse. For the patients who have their surgeries postponed their mortality increases and their survival decreases. Also, the hospitals and the healthcare systems carry higher burden of costs in the scenario of postponed and cancelled surgeries or screening/diagnostic programs as these patients will present later at more advanced stages. We believe that cancer screenings, diagnoses and surgeries in patient care pathway must be maintained at any costs to avoid a cancer crisis after the Covid-19 crisis.
About the author
Volker, Great Explorer Oncology in Alcimed’s Healthcare team in Germany
Do you have an exploration project?
Our explorers are ready to discuss it with you