What is the link between 3D printing and personalized medicine?
Among the many current healthcare transformations driven by the expansion of new technologies, the transition towards «personalized medicine » stands out because of its potential for the improvement of individual health outcomes. In this new approach, medical interventions are tailor-made to fit the needs and limitations of each individual patient, as opposed to the « one size fits all » approach that characterizes some of our traditional medical practices.
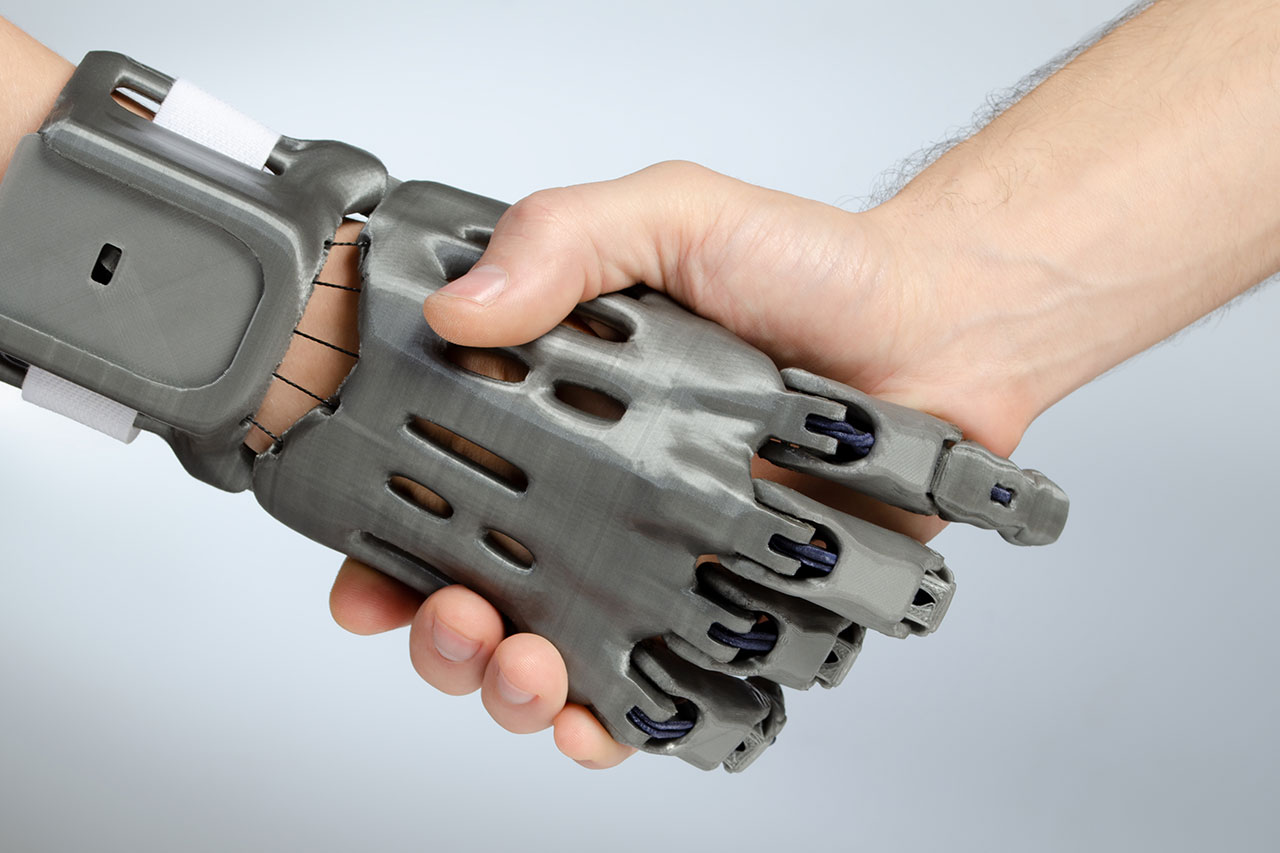
3D printing technologies allow for low-cost, high precision manufacturing of customized physical pieces. In healthcare, the application of these technologies has found fertile ground in the field of bone reconstruction surgery, in which geometrically complex devices are needed for supporting or replacing bone that has been lost or damaged beyond its capacity to heal itself.
Besides factors such as the overall health status of the patient, the location and size of the bone defect, and its cause (e.g. trauma, bone tumor resection), the success of these surgeries depends on the degree to which devices like implants and fixation plates fit with the patient’s own anatomy and the morphology of their defect. Hence the immense potential of 3D printing, by virtue of possibility it offers to control the chemistry, shape, porosity, and topography of these devices in bone reconstruction surgeries.
3D printing for preoperative planning in bone reconstruction surgeries: a multifunctional tool
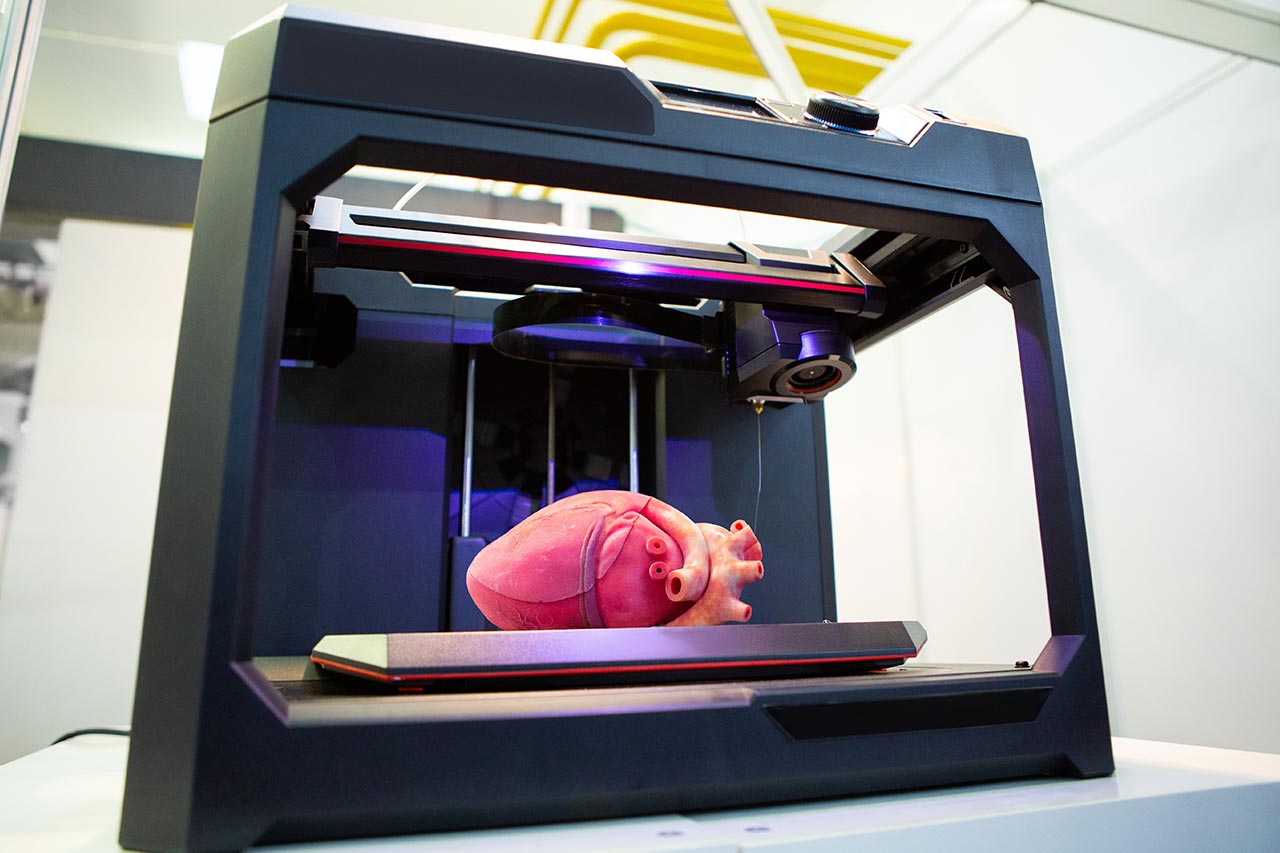
3D printing of anatomical models is already helping orthopedic surgeons to plan complex interventions. Thanks to the availability of high-resolution medical imaging technology – mainly Computed Tomography (CT) – surgeons can obtain reliable 3D digital models of their patient’s inner body structures, and then use these CAD (Computer Aided Design) files as a blueprint for printing a physical anatomical model. This approach allows surgeons to plan and discuss in advance several aspects of the surgery that are usually difficult to address before the physical intervention.
Another prominent application is the possibility to design custom-made surgical guides. These are templates that are placed over the bones to indicate the spots where surgeons will insert screws, make cuts, or adapt an implant. These custom-made guides are not only designed based on 3D-printed anatomic models of the patients, but also can be themselves manufactured using 3D printing technology.
3D printing applications for permanent implants in bone reconstruction
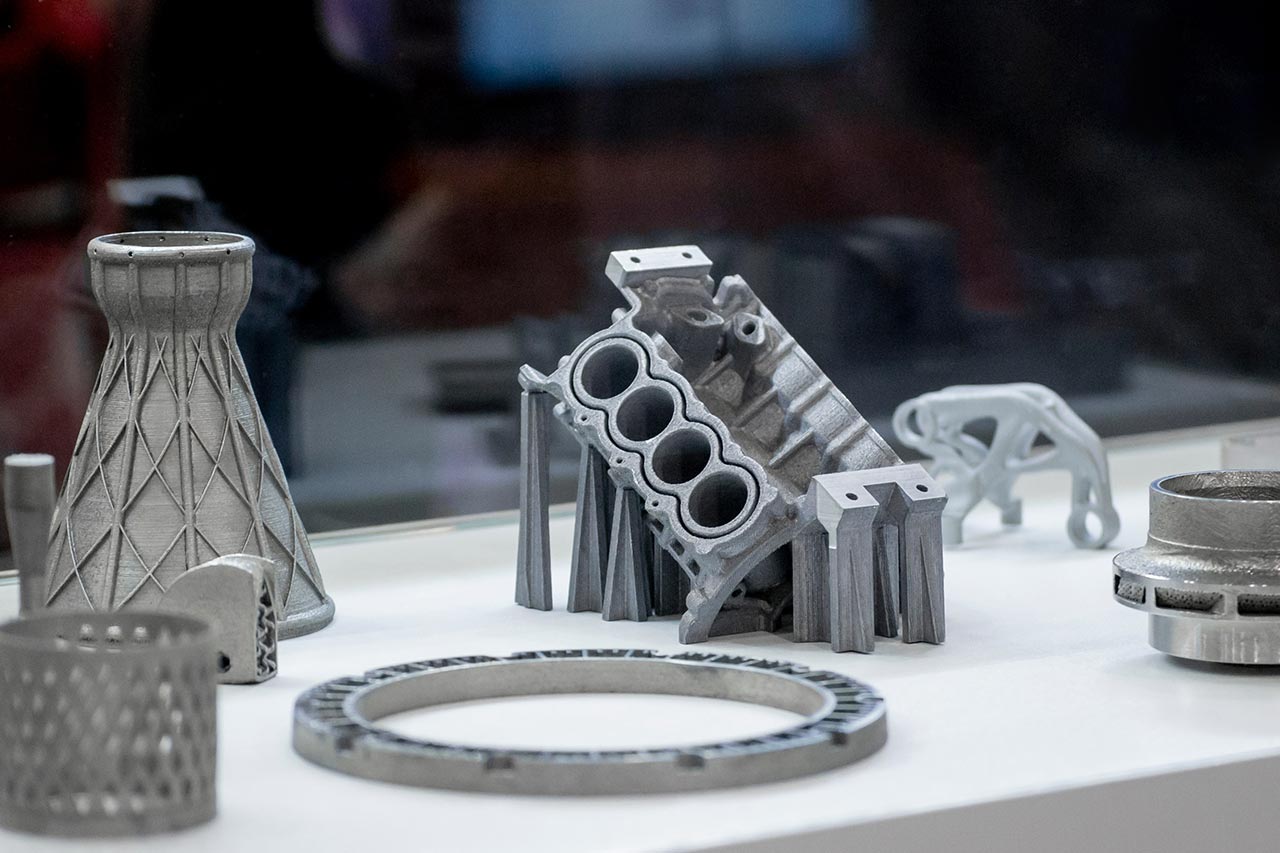
In addition to devices used for surgical planning, bone reconstruction often entails the use of permanent implants to indefinitely replace the lost or degenerated bone tissue. Some medical devices companies are already commercializing permanent 3D-printed implants such as spinal cages and acetabular cups. However, most of the 3D-printed implants commercialized today are mass produced. The prominent advantage of the use of 3D printing in these applications is not their customization to fit with individual patients’ needs, but their ability to reproduce the natural porosity of the bone.
Although relatively marginal in comparison, some companies are using 3D printing technologies to produce patient-specific implants based on the patients’ individual 3D CT-scan data. Surgeons have found this approach to be particularly significant in the reconstruction of facial and cranial bone defects, given the inadequacy of traditional manufacturing processes to reproduce the geometrical complexity of these anatomical structures. 3D printing technologies are, in addition, versatile enough to allow a wide range of possible materials and configurations, further increasing the possibilities for surgeons to choose the best solution for individual patients. A Swedish company called OSSDESIGN, for instance, is producing facial and cranial implants using ceramic tiles joined with a titanium mesh. This mosaic tile design allows for optimal load transfer to the titanium mesh, and at the same time giving space for tissue ingrowth and vascularization.
The future of 3D printing: opportunities for regenerative implants in bone reconstruction
As opposed to a permanent implant, a regenerative implant intends to replace the tissue only temporarily. This kind of implant serves as a scaffold to guide and stimulate the natural process of tissue regeneration, and ultimately will be reabsorbed by the organism by the time the defect has been reconstructed. In comparison to permanent implants, a regenerative approach has the potential to significantly reduce complications associated with the long-term implantation of foreign materials in the body (e.g. infections, host-donor disease).
In addition to being biodegradable and biocompatible (i.e. free of toxicity and inflammatory reactions), an ideal regenerative implant should also be osteoinductive: actively facilitating the recruitment or hosting of immature cells and stimulating them to develop into mature osteoblasts (bone tissue cells), which will therefore enable the natural reconstruction.
Some polymers and bio-ceramic materials used in 3D printing applications fulfill the first two properties (biodegradability and biocompatibility), but the question of osteoinductivity remains open. Surgeons are wary of the risk of implanting devices that will be reabsorbed before the actual bone growth has taken place. At this stage, there is not enough evidence to demonstrate that biodegradable implants effectively stimulate healthy bone tissue growth. Published evidence is limited to in-vitro studies, and very few experiences with live animal models have been documented, let alone with human subjects. Although limited in number, these experiences have yielded encouraging results. German researchers have, for instance, successfully reconstructed a cranial defect of around 3×3 cm using a 3D printed regenerative implant. The material used was a combination of polycaprolactone (PCL) and tricalcium phosphate (TCP).
The regenerative approach: what next steps for 3D printing technologies in bone reconstruction?
3D printing technologies are already being used for bone reconstruction, pre-operative planning, and producing permanent implants in several orthopedic and craniofacial surgery applications. Limitations of available biomaterials, mainly their low osteoinductivity, have so far hindered the evolution of these technologies towards a more “regenerative” approach.
To address these barriers, two courses of action are needed. First, accelerating fundamental research focused on developing new osteo-inductive biomaterials that could, for instance, stimulate bone tissue growth by releasing growth factors. Second, in parallel, increasing the body of evidence in favor of the safety and effectiveness of existing materials, through controlled studies in animal models and human subjects.
Although 3D printing technologies are yet to reach their maturity stage, they are already transforming the way surgeons approach bone reconstruction. At Alcimed, we are convinced that if this development pace is maintained, the coming years will bear witness to increasingly sophisticated and personalized applications of these technologies.
About the authors
David, Consultant in Alcimed’s Healthcare team in France
Céline, Project Manager in Alcimed’s Healthcare team in France