Healthcare
mRNA vaccine development in oncology: what will the future bring?
Alcimed discusses the current status of mRNA vaccines in the field of oncology and sheds a light on what the future may bring.
Next generation immune oncology does not only investigate new targets or approaches on how to target cancer cells, but also where to target them. Certain challenges are linked to systemic immune therapeutical approaches, which might be overcome using intratumoral administration of immune stimulatory drugs. In this article, we discuss advantages and hurdles of intratumoral immunotherapy, which is increasingly tested in clinical phases over the last years.
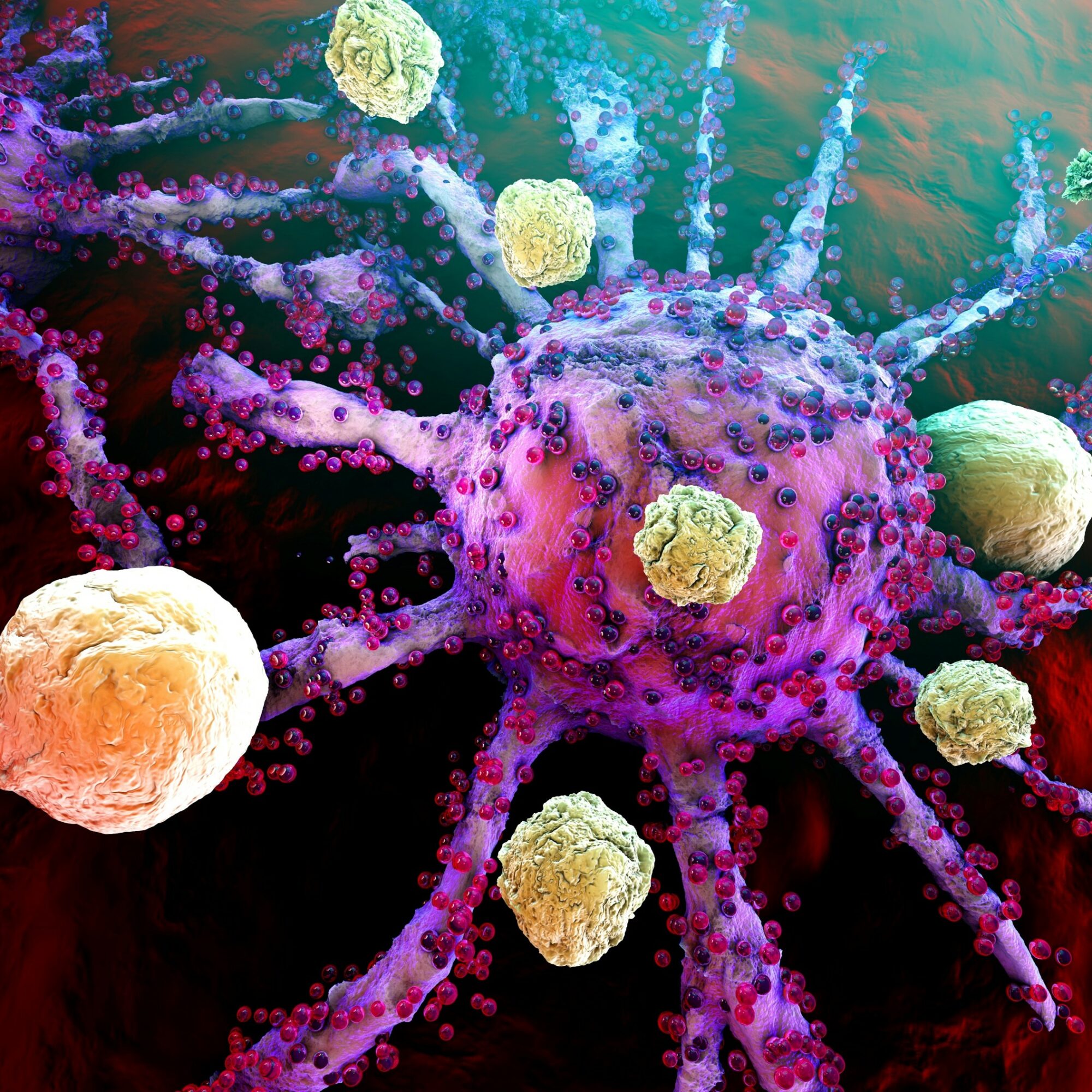
Immuno-oncology is a form of cancer treatment based on the patient’s own immune system to fight cancer cells. Advantages of immune therapy in cancer treatment are its theoretical specificity of only targeting cancer cells and the formation of a memory, which is supposed to prevent tumor reoccurrence.
In the past, different types of immune oncology therapies were designed (see Alcimed’s content about new targets of checkpoint inhibitors or CAR-T cell therapy), which all have in common that the specific drug is administered systemically. However, there a certain hurdles linked to systemic administration of immune therapeutics that are e.g. off-target effects, toxicity and antigen-escape.
Since immune oncology therapies provide durable response rates and long-term survival benefits for some cancer patients due to their unique potency relying on the full power of the human immune system, immune therapies are considered a promising therapeutical approach of cancer treatment and are basis of many innovative cancer therapies. Intratumoral immunotherapy could overcome some of the disadvantages of systemic immunotherapy and is nowadays highly investigated as encouraging alternative to systemic approaches or as supplementary therapy. In intratumoral immunotherapy, the immunostimulatory products are directly injected into the tumor lesion.
Learn more on our Oncology Exploration Center >
There are several advantages of intratumoral immunotherapy compared to the systemic delivery of immune therapeutica.
Advantage 1: Targeted, only local stimulation of the immune system at the tumor site leads to local tumor antigen release and immune cell activation. To target especially tumor cells and to not harm healthy cells, therapeutics are designed to aim especially at cancer antigens. The identification of these antigens is time consuming, however, with intratumoral immunotherapy no previous identification of tumor antigens is needed to design a therapy, since various tumor antigens are released by the tumor itself upon injection, which activates polyclonal B and T cells. Thus, in a way the tumor serves as its own vaccine. The activated immune cells attack the tumor locally at the injection site and can act systemically by travelling within the patient’s body to target secondary tumors.
Advantage 2: The activation of polyclonal immune cells to target multiple tumor antigens increases the possibility to target metastases, which often display mutated or altered tumor antigens than the primary tumor, and restricts the tumor’s ability to escape the immune response by mutating antigens. Following this thought, off-the-shelf products are able to target patient specific tumors, which significantly reduces the cost and time of pretreatment examinations, tumor analyses and planning of therapeutic strategies.
Advantage 3: The local delivery of therapeutics directly where they are needed leads not only to less off-target effects, but also to a decrease of the drug dose, which again reduces toxic effects of the given immune therapeutics and allows for combination of treatments, that otherwise might have severe side effects. In the future, patients might be treated with lower doses of therapeutics in a more potent combination, leading to less severe effects on the patients body and to a better clinical outcome.
The number of clinical trials investigating intratumoral immunotherapy increased drastically over the last years and currently 297 clinical trials are ongoing. Three intratumoral immunotherapy approaches are already approved and in use for cancer treatment:
Even though, intratumoral immunotherapy is a promising treatment approach for cancers, especially for spreading or reoccurring cancers, there are still certain challenges, which need to be tackled to improve this method further. In fact, the tumor needs to gain a sufficient size to be injected and the injection of deeper tumors requires imaging or endoscopic guidance, leading to repeated x-ray exposure and long procedure.
For injecting therapeutics into the central nervous system, surgery is necessary, which hampers repetition of injection, that might be required for optimal immune response activation.
Other questions, which might be answered in the future are how to estimate the exact dose of injected therapeutics, if only the primary tumor or also metastases should be injected and if the trauma induced by the needle or the administered anesthetics have an influence on the immune response.
Intratumoral immunotherapy offers new possibilities to increase efficacy, since the therapeutics are bioavailable locally at the tumor lesion and multiple combinations of immune-therapeutics are possible due to reduced toxicity. Additionally, intratumoral immunotherapy is assumed to overcome resistance of cancer cells to immune stimulating drugs in multiple tumor types, which are applied systemically. In the future, innovative intratumoral immune therapies will be designed that demonstrate little systemic toxicity with highly potent local activity against the tumor burden, which could be used in various indications to inhibit tumor growth, as well as to induce tumor shrinkage and to prevent tumor reoccurrence. To stay informed on the latest advances in Oncology, visit our Oncology Exploration Center!
About the author,
Volker, Great Explorer Oncology, and Frederike, Consultant in Alcimed’s Healthcare team in Germany
Have a project?
Our explorers are ready to discuss it with you